Prostate health is a natural part of aging. As men age, prostate issues, including benign prostatic hyperplasia (BPH) and prostate cancer, increase. We are committed to offering the most advanced approaches to preventing, diagnosing and treating prostate conditions.
Symptoms of Prostate Conditions
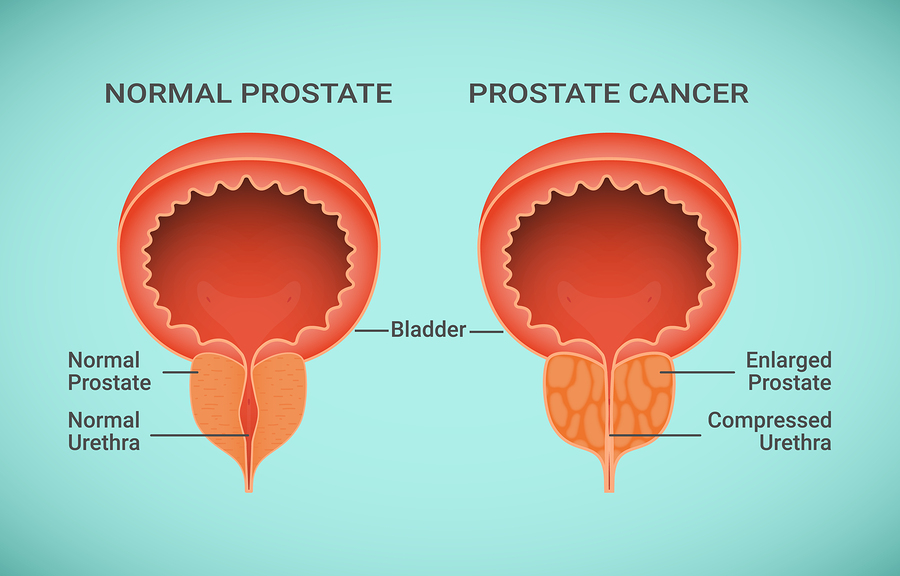
The prostate is a walnut-shaped gland under a man’s bladder. The urethra, the tube that carries urine from the bladder out of the body, passes through the prostate to the penis. A growth spurt occurs in the urethra during puberty. A second growth spurt can occur around age 50. Monitoring your prostate health grows more important as you age.
During the second growth spurt, an enlarged prostate can block urine flow through the urethra similar to a clamp around a garden hose, a condition known as an enlarged prostate or benign prostatic hyperplasia (BPH). As the bladder fights to pass urine through the blocked urethra, the bladder wall thickens, causing symptoms, including:
• increased urination frequency
• incomplete bladder emptying
• weak stream
• start and stop flow
Benign Prostatic Hyperplasia
BPH is common in men at least 50 years old. Not all men with BPH experience symptoms. When symptoms do become a problem, most cases are treated through lifestyle changes, medicine and, sometimes, surgery. Early diagnosis is the best way to stay on top of your prostate health. Tests include
Digital rectal exam (DRE) — should be a part of an annual exam and between checkups if your Dr. Bankhead suspects a problem. The doctor inserts a gloved, lubricated finger in the lower part of your rectum to feel the prostate and check for enlargement.
Prostate-specific antigen (PSA) blood test — measures blood levels of prostate-specific antigen (PSA), a substance the prostate makes. An increased amount may indicate prostate cancer.
Urine flow study — measures urine flow speed as you urinate in a special device. Slow speed could indicate BPH.
Cystoscopy — more accurately checks prostate size and collects more obstruction information. After giving you a local anesthetic, your doctor will insert a small tube called a cystoscope through the urethra opening in the penis. The tube contains a lens that allows Dr. Bankhead to see in the urethra and bladder.
A mild case of BPH may require lifestyle changes, including:
• Urinating at first urge
• Urinating regularly
• Avoiding alcohol & caffeine
• Limiting fluids in the evening
• Avoiding decongestants
• Avoiding antihistamines
• Reducing stress
Medicine- Medicines such as finasteride and dutasteride can inhibit production of hormones involved with prostate enlargement, preventing further prostate growth. Alpha 1 blockers such as terazosin, doxazosin, tamsulosin and alfuzosin can relax prostate and bladder neck muscles to improve urination. Antibiotics also may be prescribed to treat chronic prostatitis (prostate inflammation) that sometimes accompanies BPH. Dr. Bankhead may also discuss surgical options to remove obstructing prostate tissue if medicines don’t work.
Prostate Cancer
At Oklahoma Urology, your team is committed to offering you the most advanced cancer treatments available to maintain your prostate health. Our services include established approaches, as well as innovative treatments.
Prostate cancer is the most common non-skin cancer among men in the United States, particularly for men older than 50. Risk factors include:
• Being Over 65
• Family History
• Genome Changes
• Abnormal Cells
• High-Grade Prostatic IntraEpithelial Neoplasia (PIN)
Prostate cancer occurs when the cells in the prostate gland grow out of control and spread within the prostate. These cells then grow through the capsule and into neighboring organs, or break away and spread through the bloodstream and lymphatic system. Prostate cancer can be relatively harmless or extremely aggressive. Some cancers are slow growing, causing few clinical symptoms. In these cases, a patient will often die with prostate cancer rather than from prostate cancer.
Prostate Biopsy – If laboratory tests or physical examination results suggest that prostate cancer may be present, you will need to have a prostate biopsy. A biopsy is the only way to know for sure whether an individual has cancer. During a biopsy, a needle is used to remove several small pieces of prostate tissue through the rectum. These pieces of prostate tissue are examined under the microscope to determine whether cancer cells are present.
Prostatectomy – Surgery is a common treatment of Stage I, II, and sometimes Stage III cancer of the prostate. The operation used to remove the prostate cancer is called a radical prostatectomy, where the entire prostate gland with the cancer and a rim of normal tissue around it is removed. With a radical prostatectomy, a portion of the urethra is removed and the cut ends are re-attached.
Before a prostatectomy is performed, the urologist may perform surgery to take out lymph nodes to see if they contain cancer. This is called a pelvic lymph node dissection. If the lymph nodes contain cancer, the urologist may not proceed with surgery. Another form of treatment, usually hormone therapy and/or radiation therapy, is generally recommended. A pelvic lymph node dissection is most useful to prevent an unnecessary prostatectomy from being performed. It is typically recommended for patients with clinical Stage III cancer or those with higher risk Stage I or II cancer who are considering surgical treatment.
Open Radical Prostatectomy can be performed through a low abdominal incision (retropubic) or through the perineum, the area between the scrotum and the anus. With the perineal approach, one cannot simultaneously remove the lymph nodes.
Minimally Invasive Surgery has recently shown to produce better outcomes than traditional open surgery—resulting in fewer post-surgical complications, fewer blood transfusions, and shorter hospital stays. Men with prostate cancer should discuss the risks and benefits of all options.
Robitic-Assisted Radical Prostatectomy (daVinci) allows the surgeon to use controlling robotic arms that hold the surgical instruments and a camera. This technique allows Dr. Bankhead to work with a higher level of precision. The prostate is in a tightly confined area and close to nerves that affect urinary and sexual function. Avoiding damage to neighboring organs and structures is an important goal of surgery
Cryosurgery is a technique that kills cancer cells by freezing them. During this procedure, hollow steel probes, guided by ultrasound, are placed inside and surrounding the cancer. Liquid nitrogen is then circulated through the probes, freezing the cancer cells and creating a ball of ice that surrounds the cancer. A heated probe is placed near the urethra throughout the freezing process so that the urethra is protected. This procedure has some compelling advantages, such as out-patient treatment, less pain, less blood loss, and faster recovery times. Since healthy tissue is preserved in the cancer-involved organ, the procedure can be repeated if the cancer returns.
Bilateral Orchiectomy (castration) is an operation to remove the testicles. By removing the testicles, the main source of male hormones is removed and hormone levels decrease. Orchiectomy is a common treatment for patients with metastatic (Stage IV) prostate cancer who will likely require hormone therapy for life. Orchiectomy can cause side effects such as loss of sexual desire, impotence, hot flashes, and weight gain. The operation itself is relatively safe and not associated with severe complications. Because it is performed once, orchiectomy is a convenient and less costly method of hormone therapy.
TransUrethral Resection of the Prostate (TURP) is a type of prostate surgery done to relieve moderate to severe urinary symptoms caused by an enlarged prostate, a condition known as benign prostatic hyperplasia (BPH). In this procedure, the cancer is cut out of the prostate gland using a small tool that can be inserted into the prostate through the urethra.
Next Steps…
We treat prostate health diseases with the most advanced minimally invasive techniques. Call us to schedule an exam.
